Abstract
Purpose of Review
Concussion produces a variety of signs and symptoms. Most patients recover within 2–4 weeks, but a significant minority experiences persistent post-concussive symptoms (PPCS), some of which may be from associated cervical or persistent neurologic sub-system (e.g., vestibular) dysfunction. This review provides evidence-based information for a pertinent history and physical examination of patients with concussion.
Recent Findings
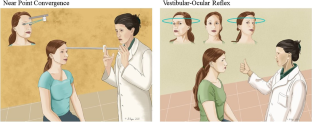
The differential diagnosis of PPCS is based on the mechanism of injury, a thorough medical history and concussion-pertinent neurological and cervical physical examinations. The concussion physical examination focuses on elements of autonomic function, oculomotor and vestibular function, and the cervical spine. Abnormalities identified on physical examination can inform specific forms of rehabilitation to help speed recovery.
Summary
Emerging data show that there are specific symptom generators after concussion that can be identified by a thorough history, a pertinent physical examination, and adjunct tests when indicated.

Similar content being viewed by others
Data availability
Not applicable.
Code Availability
Not applicable.
References
McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–47.
Maroon JC, LePere DB, Blaylock RL, Bost JW. Postconcussion syndrome: a review of pathophysiology and potential nonpharmacological approaches to treatment. Physician and Sportsmedicine. 2013;40(4):73–87.
Haider MN, Willer B, Leddy J, Ellis MJ. 2019 Multidisciplinary assessment and treatment. In: Silver JM, McAllister TW, Arciniegas DB, editors. Textbook of traumatic brain injury. 3rd ed: American Psychiatric Pub; p. 677–96.
Hyden J, Petty B. Sideline management of concussion. Phys Med Rehabil Clin N Am. 2016;27(2):395–409.
Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2014;75(suppl_4):S24–33.
Kontos AP, Jorgensen-Wagers K, Trbovich AM, Ernst N, Emami K, Gillie B, et al. Association of time since injury to the first clinic visit with recovery following concussion. JAMA Neurol. 2020;77(4):435–40.
McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–47.
Bonow RH, Friedman SD, Perez FA, Ellenbogen RG, Browd SR, Mac Donald CL, et al. Prevalence of abnormal magnetic resonance imaging findings in children with persistent symptoms after pediatric sports-related concussion. J Neurotrauma. 2017;34(19):2706–12.
Chamard E, Lichtenstein JD. A systematic review of neuroimaging findings in children and adolescents with sports-related concussion. Brain Inj. 2018;32(7):816–31.
Marshall SW, Guskiewicz KM, Shankar V, McCrea M, Cantu RC. Epidemiology of sports-related concussion in seven US high school and collegiate sports. Inj Epidemiol. 2015;2(1):13.
Nelson LD, Temkin NR, Dikmen S, Barber J, Giacino JT, Yuh E, et al. Recovery after mild traumatic brain injury in patients presenting to US Level I trauma centers: a Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) study. JAMA Neurol. 2019;76(9):1049–59.
Ellis MJ, Leddy JJ, Willer B. Physiological, vestibulo-ocular and cervicogenic post-concussion disorders: an evidence-based classification system with directions for treatment. Brain Inj. 2015;29(2):238–48.
Haider MN, Herget L, Zafonte RD, Lamm AG, Wong BM, Leddy JJ. Rehabilitation of sport-related concussion. Clin Sports Med. 2021;40(1):93–109.
Kamins J, Bigler E, Covassin T, Henry L, Kemp S, Leddy JJ, et al. What is the physiological time to recovery after concussion? Systematic review. Br J Sports Med. 2017;51(12):935–40.
Xu S, Chang JC, Chow CC, Brennan KC, Huang H. A mathematical model for persistent post-CSD vasoconstriction. PLoS Comput Biol. 2020;16(7):e1007996.
Clausen M, Pendergast DR, Wilier B, Leddy J. Cerebral blood flow during treadmill exercise is a marker of physiological postconcussion syndrome in female athletes. Journal of Head Trauma Rehabilitation. 2016;31(3):215–24.
Haider MN, Patel KS, Willer BS, Videira V, Wilber CG, Mayer AR, et al. Symptoms upon postural change and orthostatic hypotension in adolescents with concussion. Brain Inj. 2021;35(2):226–32.
Leddy J, Lesh K, Haider MN, Czuczman N, Baker JG, Miecznikowski J, et al. Derivation of a focused, brief concussion physical examination for adolescents with sport-related concussion. Clin J Sport Med. 2018;31(1):7–14.
Memmini AK, Fountaine MF, Broglio SP, Moore RD. Long-term influence of concussion on cardio-autonomic function in adolescent hockey players. J Athl Train. 2021;56(2):141–7.
Snook ML, Henry LC, Sanfilippo JS, Zeleznik AJ, Kontos AP. Association of concussion with abnormal menstrual patterns in adolescent and young women. JAMA pediatrics. 2017;171(9):879–86.
Leddy JJ, Baker JG, Merchant A, Picano J, Gaile D, Matuszak J, et al. Brain or strain? Symptoms alone do not distinguish physiologic concussion from cervical/vestibular injury. Clin J Sport Med. 2015;25(3):237–42.
Hugentobler JA, Vegh M, Janiszewski B, Quatman-Yates C. Physical therapy intervention strategies for patients with prolonged mild traumatic brain injury symptoms: a case series. Int J Sports Phys Ther. 2015;10(5):676–89.
Brodsky JR, Shoshany TN, Lipson S, Zhou G. Peripheral vestibular disorders in children and adolescents with concussion. Otolaryngology-Head and Neck Surgery. 2018;159(2):365–70.
Maestas KL, Sander AM, Clark AN, van Veldhoven LM, Struchen MA, Sherer M, et al. Preinjury coping, emotional functioning, and quality of life following uncomplicated and complicated mild traumatic brain injury. J Head Trauma Rehabil. 2014;29(5):407–17.
Iverson GL, Silverberg ND, Mannix R, Maxwell BA, Atkins JE, Zafonte R, et al. Factors associated with concussion-like symptom reporting in high school athletes. JAMA Pediatr. 2015;169(12):1132–40.
Harmon KG, Clugston JR, Dec K, Hainline B, Herring SA, Kane S, et al. American Medical Society for Sports Medicine Position Statement on Concussion in Sport. Clin J Sport Med. 2019;29(2):87–100.
Rose SC, Anderson W, Feinberg D, Ganesh A, Green L, Jaffee M, et al. Quality Improvement in neurology: concussion quality measurement set. Neurology. 2021;97(11):537–42.
Makdissi M, Davis G. Using video analysis for concussion surveillance in Australian football. J Sci Med Sport. 2016;19(12):958–63.
Zasler N, Haider MN, Grzibowski NR, Leddy JJ. Physician medical assessment in a multidisciplinary concussion clinic. The Journal of head trauma rehabilitation. 2019;Publish Ahead of Print.
Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc Sci Med. 2015;134:66–75.
Baker JG, Willer BS, Dwyer MG, Leddy JJ. A preliminary investigation of cognitive intolerance and neuroimaging among adolescents returning to school after concussion. Brain Inj. 2020;34(6):818–27.
Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2014;75(Suppl 4):S24-33.
Leddy JJ, Wilber CG, Willer BS. Active recovery from concussion. Curr Opin Neurol. 2018;31(6):681–6.
Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941–8.
Fehr SD, Nelson LD, Scharer KR, Traudt EA, Veenstra JM, Tarima SS, et al. Risk factors for prolonged symptoms of mild traumatic brain injury: a pediatric sports concussion clinic cohort. Clin J Sport Med. 2019;29(1):11–7.
Matuszak JM, McVige J, McPherson J, Willer B, Leddy J. A practical concussion physical examination toolbox evidence-based physical examination for concussion. Sports Health: A Multidisciplinary Approach. 2016;8(3):260–9.
Anzalone AJ, Blueitt D, Case T, McGuffin T, Pollard K, Garrison JC, et al. A positive vestibular/ocular motor screening (VOMS) is associated with increased recovery time after sports-related concussion in youth and adolescent athletes. Am J Sports Med. 2017;45(2):474–9.
Pertab JL, Merkley TL, Cramond AJ, Cramond K, Paxton H, Wu T. Concussion and the autonomic nervous system: an introduction to the field and the results of a systematic review. NeuroRehabilitation. 2018;42(4):397–427.
Naschitz JE, Rosner I. Orthostatic hypotension: framework of the syndrome. Postgrad Med J. 2007;83(983):568–74.
Cooke J, Carew S, O’connor M, Costelloe A, Sheehy T, Lyons D. Sitting and standing blood pressure measurements are not accurate for the diagnosis of orthostatic hypotension. QJM. 2009;102(5):335–9.
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21(2):69–72.
Kokorelis C, Slomine B, Rowe PC, Suskauer S. Screening for orthostatic intolerance in symptomatic children presenting for concussion care. Clin Pediatr. 2020;59(1):75–82.
Wieling W, Krediet CP, Van Dijk N, Linzer M, Tschakovsky ME. Initial orthostatic hypotension: review of a forgotten condition. Clin Sci. 2007;112(3):157–65.
Thompson TL, Amedee R. Vertigo: a review of common peripheral and central vestibular disorders. Ochsner J. 2009;9(1):20–6.
Fife TD, Giza C, editors. Posttraumatic vertigo and dizziness. Seminars in neurology; 2013: Thieme Medical Publishers.
Marshall CM, Vernon H, Leddy JJ, Baldwin BA. The role of the cervical spine in post-concussion syndrome. Phys Sportsmed. 2015;43(3):274–84.
Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng. 2011;133(7):071010.
Heikkilä H, Aström P. Cervicocephalic kinesthetic sensibility in patients with whiplash injury. Scand J Rehabil Med. 1996;28(3):133–8.
Luedtke K, Boissonnault W, Caspersen N, Castien R, Chaibi A, Falla D, et al. International consensus on the most useful physical examination tests used by physiotherapists for patients with headache: a Delphi study. Man Ther. 2016;23:17–24.
Hall TM, Robinson KW, Fujinawa O, Akasaka K, Pyne EA. Intertester reliability and diagnostic validity of the cervical flexion-rotation test. J Manipulative Physiol Ther. 2008;31(4):293–300.
Rubio-Ochoa J, Benítez-Martínez J, Lluch E, Santacruz-Zaragozá S, Gómez-Contreras P, Cook C. Physical examination tests for screening and diagnosis of cervicogenic headache: a systematic review. Man Ther. 2016;21:35–40.
Ogince M, Hall T, Robinson K, Blackmore A. The diagnostic validity of the cervical flexion–rotation test in C1/2-related cervicogenic headache. Man Ther. 2007;12(3):256–62.
Cheever K, Kawata K, Tierney R, Galgon A. cervical injury assessments for concussion evaluation: a review. J Athl Train. 2016;51(12):1037–44.
Osmotherly PG, Rivett DA, Rowe LJ. Construct validity of clinical tests for alar ligament integrity: an evaluation using magnetic resonance imaging. Phys Ther. 2012;92(5):718–25.
Hutting N, Scholten-Peeters GG, Vijverman V, Keesenberg MD, Verhagen AP. Diagnostic accuracy of upper cervical spine instability tests: a systematic review. Phys Ther. 2013;93(12):1686–95.
Uitvlugt G, Indenbaum S. Clinical assessment of atlantoaxial instability using the Sharp-Purser test. Arthritis Rheum. 1988;31(7):918–22.
Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002;27(2):156–9.
Kaale BR, Krakenes J, Albrektsen G, Wester K. Clinical assessment techniques for detecting ligament and membrane injuries in the upper cervical spine region–a comparison with MRI results. Man Ther. 2008;13(5):397–403.
Rainey CE. Determining the prevalence and assessing the severity of injuries in mixed martial arts athletes. N Am J Sports Phys Ther. 2009;4(4):190–9.
Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. J Korean Med Sci. 2016;31(4):479–88.
Czerniak LL, Liebel SW, Garcia GP, Lavieri MS, McCrea MA, McAllister TW, et al. Sensitivity and specificity of computer-based neurocognitive tests in sport-related concussion: findings from the NCAA-DoD CARE Consortium. Sports Med. 2021;51(2):351–65.
Broglio SP, Ferrara MS, Macciocchi SN, Baumgartner TA, Elliott R. Test-retest reliability of computerized concussion assessment programs. J Athl Train. 2007;42(4):509–14.
Lovell MR. 2006 Neuropsychological assessment of the professional athlete. Sports neuropsychology: assessment and management of traumatic brain injury. 176–90
Master CL, Master SR, Wiebe DJ, Storey EP, Lockyer JE, Podolak OE, et al. Vision and vestibular system dysfunction predicts prolonged concussion recovery in children. Clin J Sport Med. 2018;28(2):139–45.
Buckley TA, Munkasy BA, Clouse BP. Sensitivity and specificity of the modified balance error scoring system in concussed collegiate student athletes. Clin J Sport Med. 2018;28(2):174–6.
Corwin DJ, McDonald CC, Arbogast KB, Mohammed FN, Metzger KB, Pfeiffer MR, et al. Clinical and device-based metrics of gait and balance in diagnosing youth concussion. Med Sci Sports Exerc. 2020;52(3):542–8.
Buttner F, Howell DR, Ardern CL, Doherty C, Blake C, Ryan J, et al. Concussed athletes walk slower than non-concussed athletes during cognitive-motor dual-task assessments but not during single-task assessments 2 months after sports concussion: a systematic review and meta-analysis using individual participant data. Br J Sports Med. 2020;54(2):94–101.
Brodsky JR, Shoshany TN, Lipson S, Zhou G. Peripheral vestibular disorders in children and adolescents with concussion. Otolaryngol Head Neck Surg. 2018;159(2):365–70.
Haripriya GR, Mary P, Dominic M, Goyal R, Sahadevan A. Incidence and treatment outcomes of post traumatic BPPV in traumatic brain injury patients. Indian J Otolaryngol Head Neck Surg. 2018;70(3):337–41.
Sandel N, Reynolds E, Cohen PE, Gillie BL, Kontos AP. Anxiety and mood clinical profile following sport-related concussion: from risk factors to treatment. Sport Exerc Perform Psychol. 2017;6(3):304–23.
Funding
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NIH) under award number 1R01NS094444 and the National Center for Advancing Translational Sciences of the NIH under award number UL1TR001412 to the University at Buffalo, SUNY. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
John J Leddy, M Nadir Haider, James M Noble, Brian Rieger, Steven Flanagan, Barry S Willer: Conception, design, and writing of the manuscript. Jacob I McPherson, Kenneth Shubin Stein, Ghazala T Saleem, Lou Corsaro: Design and writing of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Dr. Noble is the co-founder and chief medical adviser of NoMo Diagnostics, which aims to develop an EEG-based concussion diagnostic tool; he has stock options in the company.
Dr. Rieger has an equity interest in Quadrant Biosciences (Motion Intelligence), which is working on concussion assessment and diagnostic tools, and has also received research support from the company and is Co-Chair in Brain Injury Association of New York State Concussion Initiative.
Dr. Leddy is on the Scientific Advisory boards of Neurolign, Stage Two Contract Engineering, Neuronasal, and Highmark Innovations.
Dr. Mohammad Nadir Haider is on the Scientific Advisory board of BlinkTBI and has received personal fees from BlinkCNS and Oculogica Inc.
Otherwise, the authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leddy, J.J., Haider, M.N., Noble, J.M. et al. Clinical Assessment of Concussion and Persistent Post-Concussive Symptoms for Neurologists. Curr Neurol Neurosci Rep 21, 70 (2021). https://doi.org/10.1007/s11910-021-01159-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s11910-021-01159-2




