Abstract
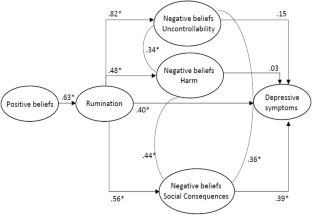
Rumination is a maladaptive emotion regulation strategy linked to depression. An intriguing question is why some people tend to use it. The metacognitive model proposes that people having positive metacognitive beliefs (“ruminating helps me cope”) are more prone to engage in ruminative processes. On the other hand, negative metacognitive beliefs (“rumination is uncontrollable”) lead to negative appraisals about rumination, increasing depressive symptomatology. Two scales assess both of these core beliefs: the Positive and Negative Beliefs about Rumination Scales (PBRS and NBRS). While they have been widely used, few studies have examined their factor structure and psychometric properties. Preliminary support has also been provided for the metacognitive model of rumination and depression, but contrary results exist about the specific contributing negative beliefs. In this study, we aimed, first, to add new evidence of the factor structure and psychometric properties of the PBRS and NBRS in a non-clinical population and, second, to test the metacognitive model using structural equation modeling (SEM). We also add the Spanish version of these scales. The participants included 427 individuals from the general population. We confirmed the one-factor structure of the PBRS and found evidence for a three-factor structure of the NBRS (uncontrollability, harm and social consequences), differing from the two-factor structure found in previous studies. SEM analyses showed that positive beliefs were associated to rumination and negative beliefs about social consequences partially mediated the relations among rumination and depression. Our findings show new data about the validity of the two scales and suggest the utility of considering a three-factor model of the NBRS.
Similar content being viewed by others
Notes
We performed the SEM analysis including the link between worry and rumination to control for the effects of worry in the mediation analyses. We used scores of each item of the PWSQ-3 as indicators for the worry latent factor. Results did not change substantially: S-B χ2 = 63.17, df = 86, p = 0.97; normed χ2 (χ2/df) = 0.73, RMSEA = 0.00; CFI = 1; SRMR = 0.07
References
Bentler, P. M. (1995). EQS: Structural equations program manual. Encino: Multivariate Software, Inc..
Berle, D., Starcevic, V., Moses, K., Hannan, A., Milicevic, D., & Sammut, P. (2011). Preliminary validation of an ultra-brief version of the Penn State Worry Questionnaire. Clinical Psychology & Psychotherapy, 18, 339–346. https://doi.org/10.1002/cpp.724.
Beshai, S., Dobson, K. S., Bockting, C. L., & Quigley, L. (2011). Relapse and recurrence prevention in depression: Current research and future prospects. Clinical Psychology Review, 31, 1349–1360. https://doi.org/10.1016/j.cpr.2011.09.003.
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., & the PROMIS Cooperative Group. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45, S3–S11. https://doi.org/10.1097/01.mlr.0000258615.42478.55.
Cohen, L. J., Ardalan, F., Yaseen, Z., & Galynker, I. (2018). Suicide crisis syndrome mediates the relationship between long-term risk factors and lifetime suicidal phenomena. Suicide and Life-threatening Behavior, 48(5), 613–623. https://doi.org/10.1111/sltb.12387.
Diez-Quevedo, L., Rangil, L., Sanchez-Planell, L., Kroenke, L., & Spitzer, L. (2001). Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosomatic Medicine, 63(4), 679–686. https://doi.org/10.1097/00006842-200107000-00021.
Hervás, G. (2008). Adaptación al castellano de un instrumento para evaluar el estilo rumiativo: la escala de respuestas rumiativas. Revista de Psicopatología y Psicología Clínica, 13(2), 111–121. https://doi.org/10.5944/rppc.vol.13.num.2.2008.4054.
Hu, L., Bentler, P. M., & Kano, Y. (1992). Can test statistics in covariance structure analysis be trusted? Psychological Bulletin, 112(2), 351–362. https://doi.org/10.1037/0033-2909.112.2.351.
Huntley, C. D., & Fisher, P. L. (2016). Examining the role of positive and negative metacognitive beliefs in depression. Scandinavian Journal of Psychology, 57(5), 446–452. https://doi.org/10.1111/sjop.12306.
Joormann, J., & Quinn, M. E. (2014). Cognitive processes and emotion regulation in depression. Depression and anxiety, 31(4), 308–315. https://doi.org/10.1002/da.22264.
Joormann, J., & Stanton, C. H. (2016). Examining emotion regulation in depression: A review and future directions. Behaviour Research and Therapy, 86, 35–49. https://doi.org/10.1016/j.brat.2016.07.007.
Kertz, S. J., Lee, J., & Björgvinsson, T. (2014). Psychometric properties of abbreviated and ultra-brief versions of the Penn State worry questionnaire. Psychological Assessment, 26(4), 1146–1154. https://doi.org/10.1037/a0037251.
Kessler, R. C., & Bromet, E. J. (2013). The epidemiology of depression across cultures. Annual Review of Public Health, 9, 119–138. https://doi.org/10.1146/annurev-publhealth-031912-114409.
Kline, R. B. (2011). Principles and practice of structural equation modelling. New York: Guilford.
Kraft, B., Jonassen, R., Ulset, V., Stiles, T., & Landrø, N. I. (2019). A prospective test of the metacognitive model of depression in previously depressed individuals. Cognitive Therapy and Research, 43, 603–610. https://doi.org/10.1007/s10608-018-9972-z.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Kubiak, T., Zahn, D., Siewert, K., Jonas, C., & Weber, H. (2014). Positive beliefs about rumination are associated with ruminative thinking and affect in daily life: Evidence for a metacognitive view on depression. Behavioural and Cognitive Psychotherapy, 42, 568–576. https://doi.org/10.1017/S1352465813000325.
Luminet, O. (2004). Measurement of depressive rumination and associated constructs. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination. Nature, theory and treatment (pp. 187–215). Chichester: Wiley.
Lyubomirsky, S., & Tkach, C. (2004). The consequences of dysphoric rumination. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination: Nature, theory, and treatment (pp. 21–42). New York: Wiley.
McEvoy, P. M., Watson, H., Watkins, E. R., & Nathan, P. (2013). The relationship between worry, rumination, and comorbidity: Evidence for repetitive negative thinking as a transdiagnostic construct. Journal of Affective Disorders, 151(1), 313–320. https://doi.org/10.1016/j.jad.2013.06.014.
Mrazek, D. A., Hornberger, J. C., Altar, C. A., & Degitar, I. (2014). A review of the clinical, economic and societal burden of treatment-resistant depression: 1996-2013. Psychiatric Services, 65, 977–987. https://doi.org/10.1176/appi.ps.201300059.
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Preita earthquake. Journal of Personality and Social Psychology, 61, 115–121.
Nolen-Hoeksema, & Watkins. (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6(6), 589–609. https://doi.org/10.1177/1745691611419672.
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x.
Papageorgiou, C., & Wells, A. (2001a). Metacognitive beliefs about rumination in recurrent major depression. Cognitive and Behavioral Practice, 8(2), 160–164. https://doi.org/10.1016/S1077-7229(01)80021-3.
Papageorgiou, C., & Wells, A. (2001b). Positive beliefs about depressive rumination: Development and preliminary validation of a self-report scale. Behaviour Therapy, 32(1), 13–26. https://doi.org/10.1016/S0005-7894(01)80041-1.
Papageorgiou, C., & Wells, A. (2003). An empirical test of a clinical metacognitive model of rumination and depression. Cognitive Therapy and Research, 27, 261–273. https://doi.org/10.1023/A:1023962332399.
Papageorgiou, C., & Wells, A. (2004). Depressive rumination: Nature, theory and treatment. Chichester: Wiley.
Papageorgiou, C., & Wells, A. (2009). A prospective test of the clinical metacognitive model of rumination and depression. International Journal of Cognitive Therapy, 2(2), 123–131. https://doi.org/10.1521/ijct.2009.2.2.123.
Pena, M., & Losada, L. (2017). Test anxiety in Spanish adolescents: Examining the role of emotional attention, and ruminative self-focus and regulation. Frontiers in Psychology, 8, 1423. https://doi.org/10.3389/fpsyg.2017.01423.
Ramos‐Cejudo, J., Salguero, J. M., & Cano‐Vindel, A. (2013). Spanish version of the meta‐cognitions questionnaire 30 (MCQ‐30). Spanish Journal of Psychology, 16, E95. https://doi.org/10.1017/sjp.2013.95.
Roelofs, J., Huibers, M., Peeters, F., Arntz, A., & van Os, J. (2010). Positive and negative beliefs about depressive rumination: A psychometric evaluation of two self-report scales and a test of a clinical metacognitive model of rumination and depression. Cognitive Therapy and Research, 34(2), 196–205. https://doi.org/10.1007/s10608-009-9244-z.
Roelofs, J., Papageorgiou, C., Gerber, R. D., Huibers, M., Peeters, F., & Arntz, A. (2007). On the links between self-discrepancies, rumination, metacognitions, and symptoms of depression in undergraduates. Behaviour research and Therapy, 45, 1295–1305. https://doi.org/10.1016/j.brat.2006.10.005.
Sandín, B., Chorot, P., Valiente, R., & Lostao, L. (2009). Validación española del cuestionario de preocupación PSWQ: estructura factorial y propiedades psicométricas. Revista de Psicopatología y Psicología Clínica, 14(2), 107–122. https://doi.org/10.5944/rppc.vol.14.num.2.2009.4070.
Schweizer, K. (2010). Some guidelines concerning the modeling of traits and abilities in test construction. European Journal of Psychological Assessment, 26(1), 1–2. https://doi.org/10.1027/1015-5759/a000001.
Spates, C. R., Pagoto, S. L., & Kalata, A. (2006). A qualitative and quantitative review of behavioral activation treatment of major depressive disorder. The Behavior Analyst Today, 7(4), 508–521. https://doi.org/10.1037/h0100089.
Sun, X., Zhu, C., & So, S. H. W. (2017). Dysfunctional metacognition across psychopathologies: A meta-analytic review. European Psychiatry: The Journal of the Association of European Psychiatrists, 45, 139–153. https://doi.org/10.1016/j.eurpsy.2017.05.029.
Trapnell, P. D., & Campbell, J. D. (1999). Private self-consciousness and the five-factor model of personality: Distinguishing rumination from reflection. Journal of Personality and Social Psychology, 76(2), 284–304. https://doi.org/10.1037/0022-3514.76.2.284.
Treynor, W., González, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. https://doi.org/10.1023/A:1023910315561.
Vilagut, G., Forero, C. G., Castro-Rodriguez, J., Olariu, E., Barbaglia, G., Astals, M., et al. (2019). Measurement equivalence of PROMIS depression in Spain and the United States. Psychological Assessment, 31(2), 248–264. https://doi.org/10.1037/pas0000665.
Watkins, E. R. (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134, 163–206. https://doi.org/10.1037/0033-2909.134.2.163.
Weber, F., & Exner, C. (2013). Metacognitive beliefs and rumination: A longitudinal study. Cognitive Therapy and Research, 37(6), 1257–1261. https://doi.org/10.1007/s10608-013-9555-y.
Wells, A. (1999). A metacognitive model and therapy for generalized anxiety disorder. Clinical Psychology & Psychotherapy, 6, 86–95. https://doi.org/10.1002/(SICI)1099-0879(199905)6:2<86::AID-CPP189>3.0.CO;2-S.
Wells, A. (2000). Emotional disorders and metacognition: Innovative cognitive therapy. Chister: Wiley.
Wells, A. (2009). Metacognitive therapy for anxiety and depression. New York: Guilford Press.
Wells, A. (2019). Breaking the cybernetic code: Understanding and treating the human metacognitive control system to enhance mental health. Frontiers in Psychology, 10, 2621. https://doi.org/10.3389/fpsyg.2019.02621.
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42, 385–396. https://doi.org/10.1016/S0005-7967(03)00145-5.
Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34, 881–888. https://doi.org/10.1016/S0005-7967(96)00050-2.
World Health Organization. (2016). Process of translation and adaptation of instruments. Retrieved from http://www.who.int/substance_abuse/research_tools/translation/en/#.
Yilmaz, A. E. (2016). Examination of the metacognitive model of depression in a Turkish University student sample. Turkish Journal of Psychiatry, 27(2), 1–9. https://doi.org/10.5080/u13505.
Funding
This study was part of a project funded by Spanish Government (grant number PSI2017–83463-R).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
All the authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cano-López, J.B., Salguero, J.M., García-Sancho, E. et al. Testing the Metacognitive Model of Rumination and Depression in Non-clinical Population: New Data about PBRS and NBRS Scales. J Psychopathol Behav Assess 43, 240–250 (2021). https://doi.org/10.1007/s10862-020-09828-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10862-020-09828-1